Top 9 Best Gifts For A Pharmacist Duties And Responsibilities
by William
Posted on 03-08-2020 04:47 AM

People interested in a career as a pharmacist should also consider the following career paths.

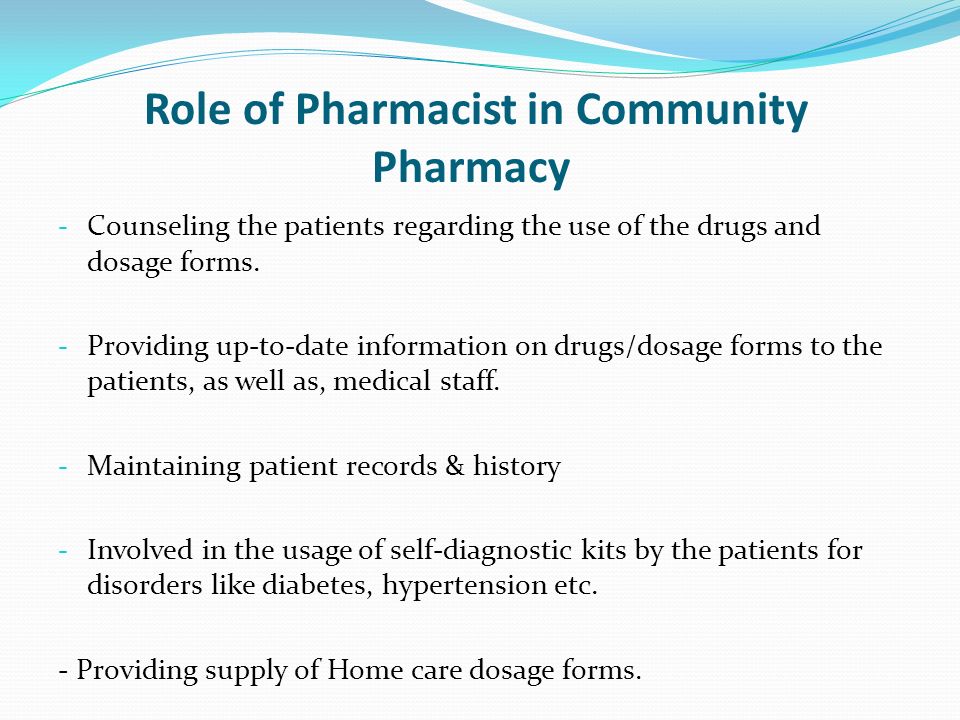
Pharmacists perform various functions; their major tasks, duties, and responsibilities are shown in the job description example below: fill patients’ prescription according to instructions given by physicians interview patients to identify conditions such as allergy or pregnancy that can be affected by intake of a drug instruct patients on the dosage and dietary requirements for drug consumption.
Pharmacy technicians fulfill a variety of administrative responsibilities in the operation of the pharmacy. They help enter and maintain customer information in account profiles, which are maintained in computer software databases. Techs also print off receipts and year-end expense totals for clients who use them for itemizing taxes. Techs also get electronic customer signatures for insurance processing at the time of purchase. Additionally, they help organize inventory and supplies, perform basic cleaning duties in the store and assist pharmacists with any other tasks that may come up.
Pharmacists earn a median yearly salary of $122,230. Pharmacy managers perform the same duties as funny pharmacist mugs pharmacist mug gifts for pharmacist s, in addition to leadership and management responsibilities. Statistical data from the bureau of labor statistics shows that pharmacists occupied more than 300,000 jobs in 2016. By 2026, this number is expected to grow 6 percent, which is as fast as the national average job growth rate.
3. Ensure Patients' Safety
From a healthcare policy and care delivery standpoint, there is an ever increasing focus on providing patient-centered care as a means of increasing the quality and safety of care. As patient care delivery evolves from episodic to longitudinal, organizations will restructure to care for patients across the continuum. This evolution will reinforce the need for team based care to ensure care coordination, patient safety, and optimal patient outcomes.
Article describes a brief outline explaining the profession of pharmacy, clinical pharmacy and the important role of a pharmacist. This profession, therefore, requires a complex and well developed set of competencies to explore one of the most health and financially rewarding careers. Pharmacy is the science and technique of preparing and dispensing drugs. This is a health profession that links health sciences with chemical sciences and it aims to ensure the safe and effective use of pharmaceutical drugs. The scope of pharmacy practice includes more traditional roles such as compounding and dispensing medications, and it also includes more modern services related to health care, including clinical services, reviewing medications for safety and efficacy, and providing drug information. The discipline of pharmacy embraces the knowledge on synthesis, chemistry and preparation of drugs, while, clinical pharmacy is more oriented to the analysis of population needs with regards to medicines, ways of administration, patterns of use and drugs effects on the patients. So, the focus of attention moves from the drug to the single patient or population receiving drugs. The experts on drug therapy are known as pharmacists that are primary health professional who optimize use of medication for the benefit of the patients. Pharmacists play an important role in helping the peoples to get the best results from their medications. Pharmacognosy studies herbs like drugs, adverse reactions and interactions; therefore, pharmacognosy is an important course of pharmacy. For that reason the pharmacists role is very important in this regard and it is important that they should understand all about correct use, adverse reactions and interactions of herb-drugs and herbs-foods.
5. Work With Patients on General Health
The nhs 'long-term plan', announced in january 2019, sets out a ten-year vision for the nhs as a way to improve access to and efficiency of services. The integration of pharmacy services with gp practices is designed to encourage patients to see their pharmacist rather than their gp for certain treatments and advice on minor ailments, as well as general health and well-being.
Developing a health care system that puts people at the center of their own care and uses all available resources as effectively as possible has become a consistent goal of most governments. Achieving this goal requires different health professionals to work in collaboration with each other to meet the health needs of patients. In order for that to happen, governments must work with all key professional groups to use all available resources of the system most effectively and, importantly, pharmacists must be recognized as the professional that coordinates drug therapy management. In addition, governments must put in place policies and a regulatory and funding environment that facilitates team-based care and acknowledges and supports the professional competencies of all health professions. These basic points were made in a white paper prepared for the alberta minister of health. This article, derived from that paper, was prepared to help pharmacists and other pharmacy organizations understand the critical steps needed for individuals and the health system to fully experience and benefit from pharmacists’ skills and services.
Equipped with a unique blend of medical know-how, communication skills and multi-tasking abilities, pharmacists are in a respected, generally well-paid position within the healthcare industry. Extending beyond the dispensing of medication at a retail drug store, the career field also has roles for consultants, researchers, and clinical pharmacists. On one hand, pharmacists earn an attractive salary and the profession shows high levels of career satisfaction. However, as with many medical-related professions, the overall job climate, shifts in government, and organization of work environments are constantly changing the role, salary and availability of jobs for pharmacists. Since no two graduates will experience the same roi (return on investment) for a pharmacy degree, it is important to weigh the following hardships and benefits before deciding to pursue the career path of a pharmacist:.
[intro paragraph] the best job descriptions provide two or three sentences that will introduce the prospective pharmacists to your company, culture, and working environment. This is where you can sell your facility to job seekers and set yourself apart from competing job listings. Pharmacist job responsibilities: serves patients by preparing medications, giving pharmacological information to multidisciplinary health care team, and monitoring patient drug therapies.
All medical doctors and nurses licensed to practice in the united states receive training on how to administer vaccines. Many medical technicians and aides also have the authority to immunize patients. Yet, as large as that health care workforce is, many american children and adults remain unvaccinated against everything from measles and mumps to chickenpox and influenza.
The review was carried out to inform the evaluation of the clinical pharmacists in general practice pilot scheme, a world leading initiative to improve health care delivery in england. Around 500 pharmacists are already working in general practice as part of the pilot, launched in july 2015.
In hospitals and health systems, pharmacy technician jobs involve patient care. Pharmacy technicians in health care facilities, such as hospitals and ambulatory clinics, often have added responsibilities in addition to filling prescriptions for patients and delivering them daily. Responsibilities include preparing sterile medications, verifying the work of other technicians, and operating pharmacy automation systems. With additional training, activities may also include obtaining medication histories, facilitating transitions of care, diversion prevention, and medication assistance programs or supply chain management. Numerous advanced or specialized technician roles exist in these settings (e. G. Pharmacy purchaser, lead pharmacy technician, and medication reconciliation technician). If you’re the kind of person who likes working directly with patients and other healthcare providers and being an active part of a medical team, pharmacy technician jobs in hospitals are a great choice.
What Does a Pharmacist Do?
In order to work as a licensed pharmacist, you must first earn a doctor of pharmacy (pharm.
 D. ) degree from a school program accredited by the accreditation council for pharmacy education (acpe). Some of the courses you may take include physics, chemistry, natural sciences, biology, and calculus. You could also learn how to interact with patients and spend up to a year working under the supervision of licensed pharmacists.
D. ) degree from a school program accredited by the accreditation council for pharmacy education (acpe). Some of the courses you may take include physics, chemistry, natural sciences, biology, and calculus. You could also learn how to interact with patients and spend up to a year working under the supervision of licensed pharmacists.
Updated february 06, 2019 no single job description covers all the 274,000-plus pharmacist positions in the united states. Practice settings for pharmacists vary widely from independently owned drugstores to nationwide grocery store chains, medical centers, military bases and marijuana dispensaries.
Education is a must, and candidates who have experience with both pharmacy and business is ideal. However, a pharmacy manager’s knowledge, experience and expertise must stand out from the rest of the candidates. What makes him different? does he have specific examples to back up his experience? hire a pharmacist who is dedicated to continuing to learn or look for business-educated individuals familiar with pharmacy nomenclature.
I. Statement of the problem the pharmacist's role is expanding beyond the traditional product-oriented functions of dispensing and distributing medicines and health supplies. The pharmacist's services of today include more patient-oriented, administrative and public health functions. There are many functions of public health that can benefit from pharmacists' unique expertise that may include pharmacotherapy, access to care, and prevention services. 1-5 apart from dispensing medicine, pharmacists have proven to be an accessible resource for health and medication information. The pharmacist's centralized placement in the community and clinical expertise are invaluable. The reexamination and integration of public health practice into pharmacological training and pharmaceutical care is essential. The encouragement of cross-training will also maximize resources and aid in addressing the work force needs within the fields of pharmacy and public health.
Updated december 16, 2018 a pharmacy benefit manager, also known as a pbm, is an organization that provides services, educational programs, and services to aid patients. They do this through affecting the behaviors of pharmacists and doctors to prescribe drugs appropriately to maximize their effectiveness. The pbm is an intermediary between insurers and other members of the healthcare industry. Because of their size, they can negotiate large customer contracts and negotiate with both pharmacies and pharmaceutical companies to get the best rates.
Pharmacist-led programs can help ease care transitions by reducing the occurrence of adverse drug events, addressing medication adherence and lowering hospital readmission rates through services such as bedside prescription transactions, counseling prior to discharge and phone consultations. In fact, a 2016 study from the cvs health research institute found that medication reconciliation programs, in which pharmacists review patients' medication regimens and provide adherence counseling during the patient's transition from hospital to home, reduced risk of hospital readmission by 50 percent, and helped avoid unnecessary health care costs.
Posted by: siobhan gilbert on august 24, 2016 in category: industry updates as prescription drug cost and usage increase in america, problems with their affordability and access are also exacerbated. This is particularly prevalent in rural areas. Though the role of the community pharmacist is expanding at a rapid rate throughout the country, no one’s role is more critical than the role of the community pharmacist in the rural united states. As the trend of younger generations moving to urban areas intensifies, rural communities tend to have a higher senior population as time goes on. Additionally, these communities have patients with more chronic illnesses. Quite often, they require multiple medications, and limited access to transportation can make it difficult for rural residents to obtain them. People may need to make long drives to the nearest pharmacy, and pharmacy hours can be more limited in rural areas, making it doubly difficult to reach a community pharmacy. Rural residents may face geographic barriers to reaching a pharmacy, such as mountains or rivers, and roads often can be impassable due to weather or seasonal closure. Public transportation options are also more limited in rural america, which poses a significant hindrance to low-income seniors.
Pharmacist Skills & Competencies
To qualify as a pharmacist, you must:
complete a general pharmaceutical council (gphc)-accredited masters degree in pharmacy (mpharm)
complete a period of one-year pre-registration training in a community pharmacy, which covers key competencies in areas such as medicines and health, personal effectiveness and interpersonal skills
pass the gphc registration assessment
meet the gphc fitness to practise requirements for registration as a pharmacist.

Soar beyond has developed some competencies and methodology for structured support to help the nhs to develop clinical pharmacists at a practice, pcn, or wider-scale level. This uses the smart (standardise and mobilise, accelerate, resources, and tools) online platform, which is designed to help with the quick deployment of clinical pharmacists to gp practices, and to develop the skills and the services they can offer in line with the practice’s needs. This is supported with an interactive tool (where pharmacists map their skillset against pre-defined competencies) and the ability to report key performance indicators (kpis). Box 3 outlines how practices can use smart to help support pharmacists, and the case study in box 4 demonstrates the smart methodology in action.
Pharmacist Role in Patient Safety
The origins and advancements of pharmacy, medicinal chemistry, and drug discovery are interwoven in nature. Medicinal chemistry provides pharmacy students with a thorough understanding of drug mechanisms of action, structure-activity relationships (sar), acid-base and physicochemical properties, and absorption, distribution, metabolism, excretion, and toxicity (admet) profiles. A comprehensive understanding of the chemical basis of drug action equips pharmacy students with the ability to answer rationally the “why†and “how†questions related to drug action and it sets the pharmacist apart as the chemical expert among health care professionals. By imparting an exclusive knowledge base, medicinal chemistry plays a vital role in providing critical thinking and evidence-based problem-solving skills to pharmacy students, enabling them to make optimal patient-specific therapeutic decisions. This review highlights the parallel nature of the history of pharmacy and medicinal chemistry, as well as the key elements of medicinal chemistry and drug discovery that make it an indispensable component of the pharmacy curriculum.
The covid-19 pandemic has placed a spotlight on the vital role of pharmacists within healthcare teams and their ability to provide a wide range of patient care services. Recent developments are advancing provider status for pharmacists and show the potential for long-term changes within the profession. “momentum for provider status has been increasing for a while now. At this point, it’s really more a question of when the government is going to act to change sections of the social security act to allow pharmacists to obtain provider status,†says ken maxik, mba, mbb, fache, rph, completerx vice president, support services. Maxik adds that a major hurdle for the profession is that pharmacists are unable to bill the centers for medicare and medicaid services (cms) under part b for services unless they’re under a recognized provider’s number.
Pharmacists are dynamic, patient-oriented professionals committed to fulfilling the health care needs of their patients. Pharmacy is a profession that is expanding in new directions to meet the health care needs of all canadians. Currently, there is a movement beyond the traditional compounding and dispensing of medication towards a more professional advisory and primary health care role.
Prescription drugs are a key component in the healthcare rural americans receive. Pharmacies and pharmacists, in particular, play a critical role in dispensing these medications, educating patients, and ensuring patient safety. However, rural community pharmacies face many challenges to stay open, including low-volume purchasing, slim profit margins, unfavorable insurance practices, a limited pharmacy workforce, and the slow growth of many.
Traditional attempts to summarise the role of the pharmacist have been ‘product focused’ i. E. Through the medicine (usually its manufacture and supply) and the associated information provided. It could therefore be said that the primary role of the pharmacist was to be an expert in medicines. Now the focus of what the role should be for many has moved to that of caregiver — the pharmacist is committed to person-centred care by ensuring the high-quality use of medicines. This encompasses effectiveness, safety and patient experience. The pharmacist may also have generic roles as an educator, manager, mentor, business/service developer, leader, researcher etc. The proportion of additional roles undertaken will depend on the location of their practice, experience, competencies, interests and other factors. The role may not need to be directly patient-facing to be person-centred.
Nhrmc is committed to utilizing a team-centered and value-focused approach to provide quality healthcare to all patients. Our institution has taken initiatives to reduce readmissions and improve patient outcomes by expanding the role of inpatient and outpatient pharmacists. The teamwork, communication, and collaboration among inpatient and outpatient pharmacists are what differentiate nhrmc and.
Pharmacists, also known as chemists ( commonwealth english ) or druggists (north american and, archaically, commonwealth english), are health professionals who specialize in the use of medicines , as they deal with the composition , effects, mechanism of action and proper and effective use of drugs. Using knowledge of the mechanism of action of drugs, the pharmacist understands how they should be used to achieve maximum benefit, minimal side effects and to avoid drug interactions. Pharmacists undergo university or graduate-level education to understand the biochemical mechanisms and actions of drugs, drug uses, therapeutic roles, side effects, potential drug interactions , and monitoring parameters. This is mated to anatomy, physiology, and pathophysiology. Pharmacists interpret and communicate this specialized knowledge to patients, physicians , and other health care providers.
Background: The Evolving Role of the Pharmacist
Team-based cardiovascular care, including the use of clinical pharmacists, can efficiently deliver high-quality care. This joint council perspectives paper from the cardiovascular team and prevention councils of the american college of cardiology provides background information on the clinical pharmacist’s role, training, certification, and potential utilization in a variety of practice models. Selected systematic reviews and meta-analyses, highlighting the benefit of clinical pharmacy services, are summarized. Clinical pharmacists have a substantial effect in a wide variety of roles in inpatient and ambulatory settings, largely through optimization of drug use, avoidance of adverse drug events, and transitional care activities focusing on medication reconciliation and patient education. Expansion of clinical pharmacy services is often impeded by policy, legislation, and compensation barriers. Multidisciplinary organizations, including the american college of cardiology, should support efforts to overcome these barriers, allowing pharmacists to deliver high-quality patient care to the full extent of their education and training.
Use of Pharmacists to Address Limitations of Technology
Pharmacists, particularly those involved in tg health care in hospital settings as part of an integrated team, should be familiar with clinical guidelines recommending laboratory monitoring of tg patients on cross-sex hormone therapy. They should also have access to laboratory findings to explore any discrepancies in values. However, this raises a very important question: “what gender-specific reference intervals are ‘normal' for each patient?†this issue was addressed in a small study comparing laboratory results from 55 tg females on hormone therapy with 20 male and 20 female cisgender subjects (i. E. , individuals whose gender identity or expressions align with assigned sex at birth). 78 the study found that hemoglobin, hematocrit, and low-density lipoprotein cholesterol laboratory values resembled those found in cisgender females (p<0. 005) while alkaline phosphatase, potassium ion, and creatinine resembled those values found in cisgender males (p<0. 05). On the contrary, triglyceride levels were higher (p<0. 005) than either cisgender male or female groups. Discrepancies in creatinine clearance are particularly important since renal function often impacts dosing protocols of many agents. These findings have important implications in that almost half of diagnostic errors occur at the level of the laboratory testing (e. G. , failure to order, report, and follow-up laboratory results). 79 due to limitations in laboratory reference values, it is imperative that reference ranges be established for tg male or tg females to avoid unnecessary evaluations, misdiagnoses, or unwarranted therapy.
Pharmacists' Role in Error Reporting and Feedback
Pharmacists have a central role in ensuring medication safety across the continuum of care. The complexity of the medication prescribing and delivery processes can make it difficult to prove the beneficial effect of pharmacists on adverse outcomes directly, but pharmacist involvement has been shown to reduce errors, improve prescribing practices, and enhance patient monitoring across settings. For example, a cluster-randomized trial of pharmacist involvement in medication management planning on hospital admission showed a dramatic reduction in medication errors within the first 24 hours of hospitalization. A meta-analysis of 13 studies of pharmacist interventions at transitions of care estimated a 37% reduction in medication errors and a decrease in emergency department visits after hospital discharge. A recent randomized controlled trial of a pharmacist-led intervention in primary care practices in the united kingdom tested an intervention bundle comprised of review of electronic medical records, prescriber feedback, education on error reduction, and support for improving local safety systems. This bundle of practices resulted in significant increases in appropriate prescribing and monitoring practices for specific error-prone situations, such as elderly patients taking loop diuretics or angiotensin-converting enzyme inhibitors. Despite these generally positive results, many health systems have found it difficult to hire enough qualified pharmacists, either because of a shortage in the available pharmacists or the costs of implementation. Given the latter factor, further studies that consider the return-on-investment of pharmacist-led safety programs should be considered.
The role of the pharmacist has evolved since the days when you would pop into a pharmacy to buy cough medicine or get a prescription fulfilled. Now pharmacists can sell dozens of medications with proper advice, including the morning-after pill , thrush medication, and eye drops. Some pharmacists can also carry out health checks, testing for chlamydia and assess your likelihood of getting brittle bone disease. It's all there at your local pharmacy.
When it comes to medical care, no one on the hospital team understands medications and the role they play in a patient's body like the pharmacist. While pharmacists have historically been responsible for dispensing prescriptions, 21st century hospital pharmacists often assume a more hands-on clinical role in patient care.
In december 2019, a respiratory illness due to a novel coronavirus, sarsâ€covâ€2, was first identified in china. 1 the respiratory illness due to sarsâ€covâ€2, termed covidâ€19, is now a worldwide pandemic and has been identified in 183 countries and 266 073 people. 1 common symptoms of covidâ€19 include cough, shortness of breath, and fever; disease ranges in severity from asymptomatic infection, mild disease (in 81% of patients), to pneumonia, respiratory failure, and death. 2 worldwide there have been 11 184 deaths associated with covidâ€19, and the current data suggest that the elderly or those with comorbid conditions such as hypertension or diabetes are at the highest risk for mortality. 1 , 3 although intensive precautions to limit spread in china appear to be decreasing the number of new cases within china, the global number of infections continues to rise rapidly. 1 identification of covidâ€19 in the united states has been challenging, given insufficient availability of testing supplies. 4 although, supplies and testing are starting to increase significantly in the united states, among countries affected by covidâ€19, the united states has among the lowest testing per capita. 5 , 6 the inability to test widely and quickly has hindered our ability to characterize the epidemiology of the disease, prevent further spread, and ensure the optimal use of other limited resources such as personal protective equipment (ppe) and medication therapy. Pharmacists play an essential and unique role within the healthcare team to optimize patient care during this covidâ€19 pandemic.
As people’s health care needs continue to change, pharmacists have become one of the most accessible health care professionals. But what exactly is their role? and what can you expect from your pharmacist?.
Columbia, south carolina us pharm. 2015;40(3):hs8-hs12. Abstract: an operating-room (or) pharmacist is a great asset to the perioperative team. The establishment of nurse-pharmacist teams in the perioperative area can reduce the incidence of adverse drug events because the pharmacist can review orders prior to administration. Or pharmacists can have a significant effect on hospital compliance with surgical care improvement project measures. Several regulatory compliance processes can be monitored and addressed daily by or pharmacists. Initiating new processes and standardizing anesthesia drug trays can decrease medication errors, improve organization of anesthesia medications, and encourage safe injection practices. A key role of the or pharmacist is to manage narcotic dispensing and reconciliation processes that inhibit drug diversion. Inclusion of a pharmacist on the multidisciplinary or team should be standard practice in all hospitals.
Jennifer leclaire, monster contributing writer with more pharmacists growing weary of day-in and day-out pill-dispensing duties, clinical pharmacy is attracting druggists who want to play a vital role on the healthcare team. Unlike many other pharmacists, clinical pharmacists are directly involved in patient care. The average hospital-based clinical pharmacist makes rounds with doctors, suggests drug therapies and monitors patient responses. In ambulatory care clinics, clinical pharmacists often determine formularies, and in industrial settings, they may conduct cost-benefit analyses on medications or educate insurance companies about new drugs.
Search
Categories
- Songwriter
- Resident Care
- Retirement
- Runner
- Sailor
- Helmsman
- Grammar Police
- Flight Attendant
- Fisher
- Entertainer
- Editor
- Daily Nutritinionist Facts
- Cyber Security
- Crusader
- Criminology
- Coworker
- Clinical Specialist
- Clinical
- Optometrist
- Logistician
- Magistrate
- Manicurist
- Marines
- Marketer
- Occupation
- Observer
- Officer
- Oncologist
- Painter
- Lifeguard
- Infopreneur
- Nanny
- Cartographer
- Expediter
- ESL Teacher
- Comedian
- Estimator
- Flagger
- Discjokey
- Driving
- Electrologist
- Fumigator
- Erector
- Driller
- Educator
- Dressmaker
- Forensic
- Legislator
- Harvester
- Cooker
- Inspector
- Hacker
- Civil Law
- Employer
- Enologist
- Endocrinologist
- Freelancer
- Enrobing
- Fabricator
- Forecaster
- Clown
- Criminologist
- Collector
- Docent
- Concierge
- Conservator
- Digger
- Dishwasher
- Drafter
- Donor
- Controller
- Communication
- Compounder
- Civil
- Clone
- Doctor
- Cinematographer
- Chiropractor
- Rugger
- Bailbondsman
- Jailer
- Deckhand
- Bellman
- Social Worker
- Babysitter
- Reporter
- Trainer
- Agent
- Embroiderer
- Sociologist
- Pharmacist
- Paramedic
- Insurance
- Teller
- Actuary
- Bailiff
- Coordinator
- Carpenter
- Cleaner
- Academic Dean
- Judge
- Boilermaker
- Clerk
- Apprentice
- Secretary
- Author
- Embalmer
- Hiker
- Cooking
- Deputy Sheriff
- Landscaper
- Photographer
- Pediatrician
- Pilot
- Teacher
- Archivist
- Toolmaker
- Singer
- Racer
- Accounting
- Mentor
- Vice President
- Detective
- Waiter
- Florist
- Broker
- Consultant
- Geographer
- Adjuster
- Auctioneer
- Researcher
- Cardiologist
- Marketing
- Interviewer
- Custodian
- Curator
- Caretaker
- Butcher
- Martial Arts
- Ghostbuster
- Mayor
- Machinist
- Innkeeper
- Mediator
- Conductor
- Demonstrator
- Programmer
- Cabinet Maker
- Planner
- Patient
- Copywriter
- Mechanic
- Surfer
- Employee
- Tour Guide
- Fisherman
- Surveyor
- Manager
- Supervisor
- Appraiser
- Police
- Filmmaker
- Woodworker
- Lecturer
- Inventor
- Liaison Officer
- Laborer
- Translator
- Janitor
- Tailor
- Debater
- Climber
- Politician
- Journalist
- Dietitian
- Firefighter
- Adjudicator
- Producer
- Housekeeper
- Entrepreneur
- Bartender
- Barista
- Hairstylist
- Banker
- Baker
- Electrician
- Therapist
- Astronaut
- Professor
- Architect
- Announcer
- Veterinarian
- Scientist
- Investigator
- Dispatcher
- Creative Writing
- Engineer
- Librarian
- Wanker
- Psychology
- Lieutenant
- Realtor
- Pastor
- Biker
- Nutrition
- Dancer
- Musician
- Gardener
- Farmer
- Counselor
- Boss
- Director
- Dentist
- Lawyer
- Nurse
- Accountant
- Coach
- Advisor
- Beekeeper
- Administrator